
Dry eye disease is a common condition that coincides with a variety of signs, symptoms and environmental conditions that all mean it has high potential for being overlooked. It’s prevalence is high with studies ranging from 5-35% but despite this, and despite its potential for significant quality of life impacts, we currently don’t have a clear path to effective management.
To chart this path is the charge of the Tear Film and Ocular Surface Society. With the second iteration of Dry Eye Workshop (DEWS) Report published in July 2017, a worldwide collaborative effort has been made to define and assist in management. The amount of research in this area has exploded with the number of papers cited jumping since the first report.
DEWS II has covered a lot of ground in the basic science of the causes and factors that result in developing dry eye disease. A key new point is that dry eye disease often causes nerve damage which contributes to symptoms, even more so than inflammation does. Management is still stepwise but must be more personalised to the contributing factors in each case. Many treatment recommendations have not changed significantly from the earlier report. This may be due to the often inconsistent link between the symptom felt and the signs observed of dry eye disease. Evidence of significant improvements with treatments in signs without symptoms, or vice versa, makes research in this area difficult.
One of the priorities of the new report is an update of the definition of the disease. Dry eye is defined in the report as a multifactorial disease of the ocular surface, characterized by a loss of homeostasis of the tear film and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiologic roles.
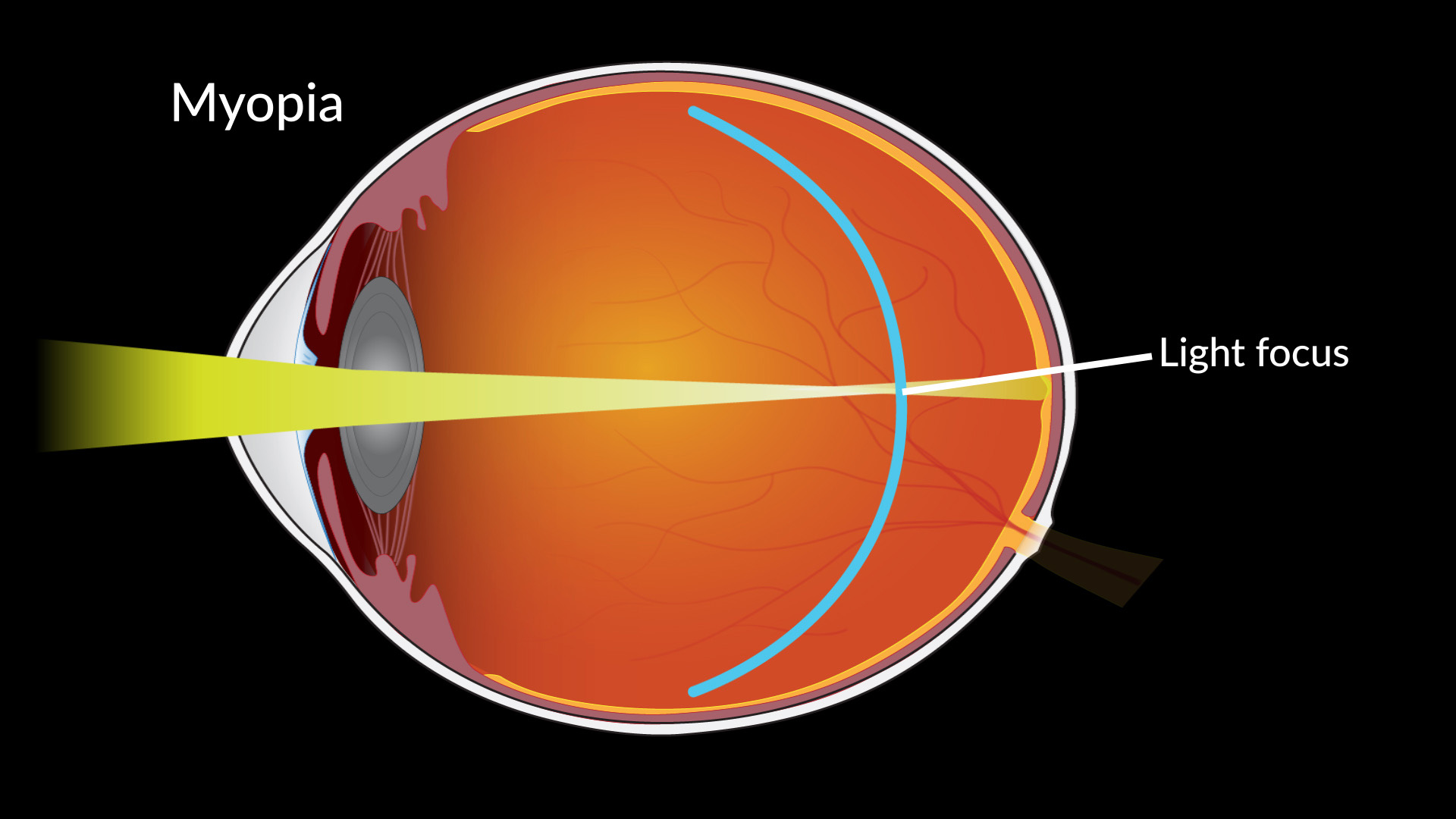
The updated understanding of the disease has condensed the previous 3 layer model of the tear film to a 2 layer model: a surface oil layer and a water-mucous layer. Dry eye disease can be a result of a problem with either layer 1) Aqueous deficient or 2) Evaporative and making the distinction is an important step in appropriate management. Once this distinction has been made, tear film osmolarity is the single most reliable objective metric of dry eye disease with highest correlation to severity. This technology is available at Innovative Eye Care. We can also measure the key metrics of the 2 forms of the disease: non-invasive tear meniscus height for aqueous deficient and non-invasive tear breakup time for evaporative dry eye disease.
Where treatment has greatly changed is in the increasing role of the health of the eyelids on dry eye disease and also the use of scleral contact lenses.
Dry eye management must address treating any blepharitis and meibomian gland disease if they are present. Additionally, controlling Demodex mites is now an established factor to look at in treating dry eyes. We at Innovative Eye Care have a comprehensive range of DEWS II validated treatments for eyelid disease from Blephex, Blephadex, Oust Demodex, Intense Pulse Light, heat masks, Sterilid, Optimel Medical Manuka Honey and Ocusoft.
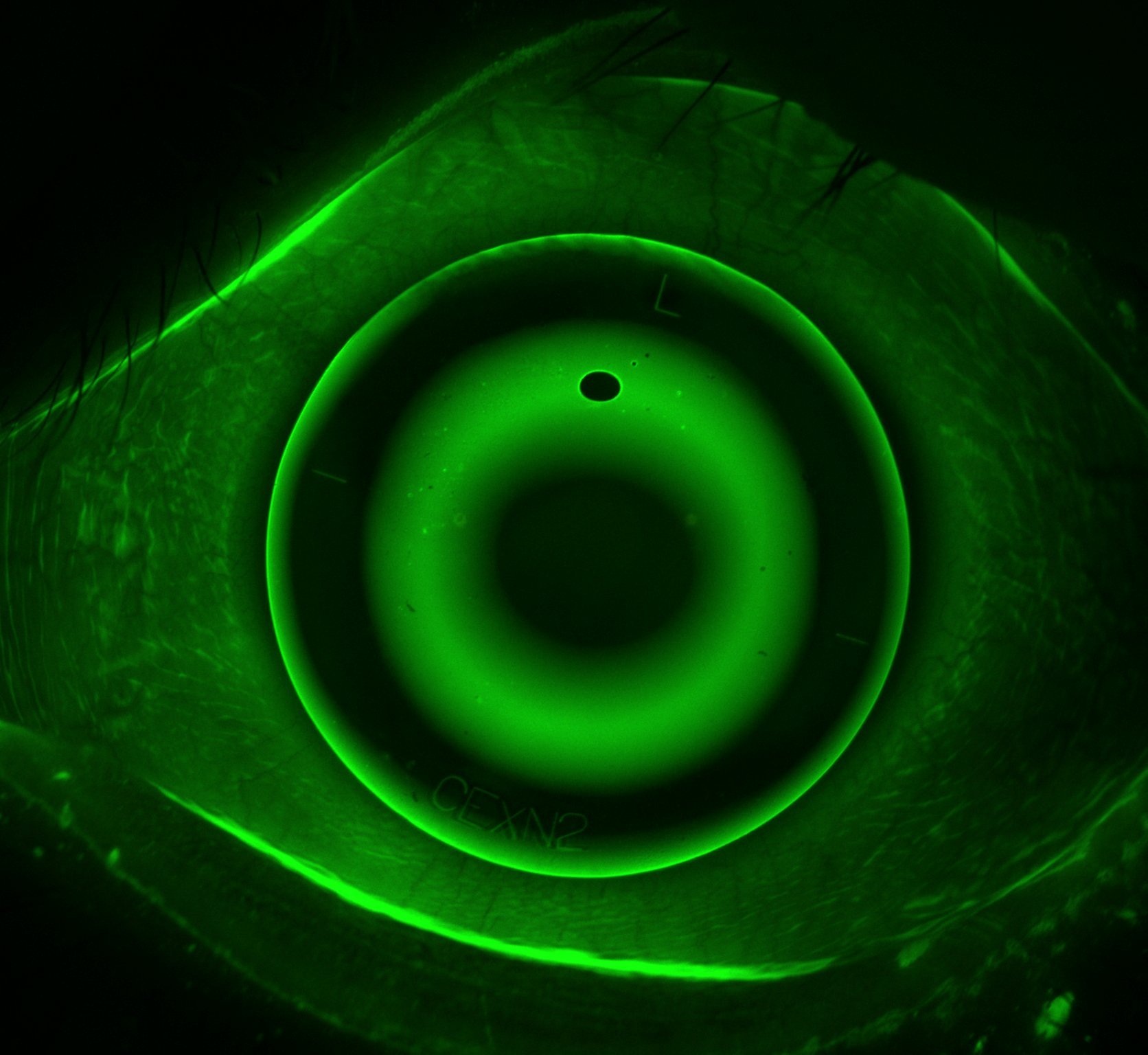
Advances in scleral contact lens fitting techniques have allowed for the greater use of comfortable, large diameter rigid lenses capable of holding a layer of tears between the lens and the eye all day long. This is a fundamental new technology for managing dry eye disease. Also, the more temporary use of soft disposable lenses can be used in a bandage role to rehabilitate the eye’s surface.
Several new drugs are available that target inflammatory and mucous secretion approaches but these are not available in Australia. This may change in the future but that timeline is unknown.
Lubricant drops help but can’t mimic the complex system of water, oils and mucous together with electrolytes and proteins that our tears are. They can be a bother to instill all day long when our eye glands would normally be producing these parts continuously.
If you are having trouble with dry eyes or eye discomfort that has not been diagnosed and in particular if you also score greater than 23 on the following questionnaire, then we at Innovative Eye Care may be able to help.
Appendix 1: OSDI Dry Eye Questionnaire

From: Schiffman, R.M., Christianson, M.D., Jacobsen, G., Hirsch, J.D., and Reis, B.L. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000; 118: 615–621
Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118(9):1264–1268.
Tomlinson, A., Khanal, S., Ramaesh, K., Diaper, C., and McFadyen, A. Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci. 2006; 47: 4309–4315
DEWS II available at http://www.theocularsurfacejournal.com/article/S1542-0124(17)30120-9/fulltext







%20(1).png)




















